Abstract
Background. Ara-c based chemo-immunotherapy followed by autologous stem cell transplantation (ASCT) is the most effective approach in young mantle cell lymphoma (MCL) patients, though few if any patients are cured. Recent data indicate that subsequent Rituximab maintenance (RM) prolongs PFS and OS (Le Gouill NEJM 2017). Lenalidomide is an oral agent effective in MCL, considered suitable for prolonged maintenance programs, but has never been tested in this setting. The FIL MCL0208 trial (NCT02354313) is a prospective, international randomized, phase III trial, comparing Lenalidomide maintenance (LM) vs observation (OBS) after an intensive Ara-c containing chemo-immunotherapy (R-HDS) program, followed by ASCT in previously untreated MCL patients.
Patients and Methods. Adult patients aged 18-65 years, with advanced stage MCL without clinically significant comorbidities were enrolled. Patients received 3 R-CHOP-21, followed by R-HDS i.e. R-high-dose Cyclophosphamide (R-HD-CTX) (4g/m2), 2 cycles of R-high-dose Ara-C (R-HDAC) (2g/m2 q12x3 d). CD34+ cells were collected after the first course of R-HDAC. The conditioning regimen for ASCT was BEAM. After ASCT, responding patients were randomized between LM (15 mg days 1-21 every 28 days) for 24 months or observation. Primary endpoint analysis was scheduled at the occurrence of the 60th PFS event in the randomized population, which occurred on June 20th, 2017 and data were analyzed for the present abstract on March 3rd 2018.
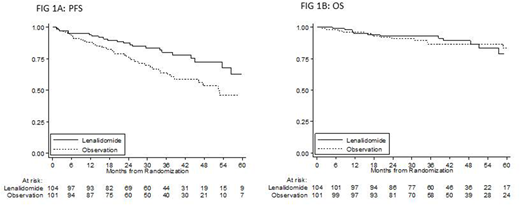
Results. Three-hundred three patients were enrolled from May 2008 to August 2015 by 48 Italian and 1 Portuguese Center. Three patients were excluded after central histological review. Median age was 57 years (IQR 51-62), M/F ratio 3.6/1. Ninety-two percent of patients had stage IV, 33% bulky disease (>5 cm), 33% elevated LDH, and 75% BM infiltration. Ki67 ≥30% was observed in 32%, MIPI was low (L) in 54%, intermediate in 31% and high (H) in 15% of patients. MIPI-c was L in 49%, low-intermediate (LI) in 29%, high-intermediate (HI) in 14%, H in 9%. Nine percent had blastoid variant. Fifty-two (17%) patients interrupted treatment before randomization (8 toxic deaths, 1 death for car accident, 24 progressions and 19 toxicity/refusals). On an ITT basis, the R-HDS + ASCT program induced 78% of CR, 7% of PRs, 10% of PD, 3% of toxic deaths (TRM) and 2% NA. Median follow-up (mFU) from inclusion was 51 months. Three years PFS and OS for the enrolled population were 67% and 84%, respectively. Of 248 patients who received ASCT, 205 were randomized either to LM (n=104) or OBS (n=101) and 43 (17%) were not because of: lack of response (8), refusal/PI decision/delay (8), unresolved infections (3) and inadequate hematopoietic recovery (24). Feasibility and efficacy were assessed on an ITT basis while toxicity was analyzed on subjects receiving at least one Lenalidomide dose. In the LM arm, 53 out of 104 patients did not start or complete the planned maintenance because of death (2), AE (26), PD (7), still ongoing (2), other causes (16). In the OBS arm 32 patients did not complete the observation phase because of death (1), AE (1), PD (20), still ongoing (10), other causes (1). Overall 28% of patients received less than 25% of the planned Lenalidomide dose. Despite suboptimal exposure to study drug, with a mFU from randomization of 35 months, 22 PFS events were recorded in the LM cohort vs 38 in the OBS arm, resulting in a 3y-PFS of 80% (95% CI; 70%-87%) in the LM arm vs. 64% in the OBS arm (95% CI; 53%-73%), stratified HR 0.51; 95% CI 0.30-0.87; p=0.013 (Fig 1A). OS was superimposable in the two arms: 93% vs 86%, stratified HR 0.96, 95% CI 0.44-2.11, p= 0.91 (Fig1B). Two deaths were observed in the LM arm due to pneumonia and thrombotic thrombocytopenic purpura and one in the OBS arm due to pneumonia. Grade 3-4 hematological toxicity was seen in 63% of patients in LM vs 11% in the OBS arm with 59% vs 10% of patients experiencing granulocytopenia. Non-hematological grade 3 toxicity was comparable in the two arms except grade 3-4 infections (11% vs. 4%; Fisher's p=0.10). Second cancers occurred in 7 patients in the LM and 3 in the OBS arm (Fisher's p=0.20).
Conclusions. Results from the MCL0208 trial indicate that LM has a clinically meaningful anti-lymphoma activity in MCL. However, the applicability of LM has some limitations in the context of patients undergoing intensified chemoimmunotherapy. Overall these data support the use of a maintenance regimen after ASCT in young MCL patients.
Ladetto:Roche: Honoraria; Celgene: Honoraria; Acerta: Honoraria; Jannsen: Honoraria; Abbvie: Honoraria; Sandoz: Honoraria. Di Rocco:Roche: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees. Rossi:Novartis: Honoraria; Jazz: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Teva: Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses; Amgen: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses; Janssen: Membership on an entity's Board of Directors or advisory committees, Travel expenses; Roche: Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria; Mundipharma: Honoraria; Sandoz: Honoraria; Seattle Genetics: Research Funding; Alexion: Other: Travel expenses. Chiappella:Janssen: Membership on an entity's Board of Directors or advisory committees, Other: lecture fees; Roche: Other: lecture fees; Teva: Other: lecture fees; Nanostring: Other: lecture fees; Amgen: Other: lecture fees; Celgene: Membership on an entity's Board of Directors or advisory committees, Other: lecture fees. Rusconi:Celgene: Research Funding. Gomes da Silva:Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: lecture fees; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: lecture fees, Institution's payment for consultancy, Travelling support; Celgene: Other: Travelling support; BMS: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: lecture fees; Roche: Other: Institution's payment for consultancy, Travelling support; Gilead Sciences: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: lecture fees, Research Funding. Vitolo:Takeda: Speakers Bureau; Sandoz: Speakers Bureau; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Gilead: Speakers Bureau. Martelli:Sandoz: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; F. Hoffman-La Roche: Membership on an entity's Board of Directors or advisory committees; Servier: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Mundipharma: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal